CDC's Decision to Remove COVID-19 Vaccine from Federal Schedule
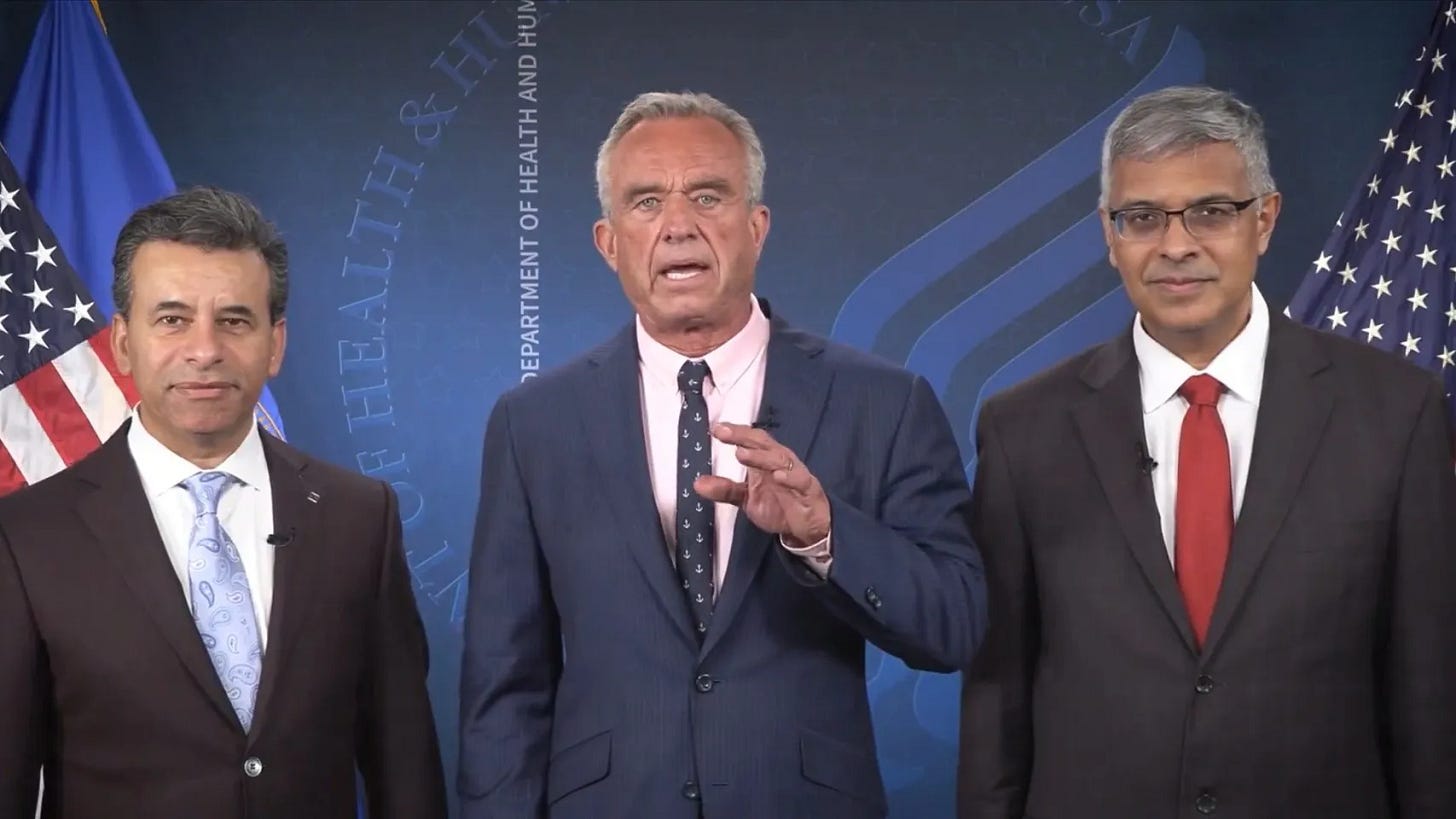
The Centers for Disease Control and Prevention’s (CDC) decision to remove the COVID-19 vaccine from the federal immunization schedule represents a monumental shift in public health policy, one that echoes years of persistent advocacy by Robert F. Kennedy Jr. This unprecedented move has reverberated across the medical community, sparking intense debates about vaccine safety, efficacy, and the foundational principles of public health in the United States.
Far more than a bureaucratic adjustment, this decision touches on critical issues: the sanctity of informed consent, the outsized influence of pharmaceutical corporations, and the pressing need for transparent, rigorous scientific standards. Vaccines have historically been a triumph of medicine, saving millions from diseases like smallpox and polio.
Yet, the COVID-19 experience has laid bare systemic flaws—flaws that Kennedy and his supporters have long highlighted. This is not a wholesale rejection of immunization but a clarion call for improved science, heightened accountability, and respect for individual autonomy in medical decision-making.
Who Is Robert F. Kennedy Jr.?
Robert F. Kennedy Jr., a member of one of America’s most iconic political families, initially gained prominence as an environmental lawyer. His decades-long career included notable work with the Natural Resources Defense Council and the founding of the Waterkeeper Alliance, where he fought to protect ecosystems and hold polluters accountable.
However, in the early 2000s, his trajectory shifted dramatically after encounters with parents who believed vaccines had harmed their children. This led him to investigate thimerosal, a mercury-based preservative once used in childhood vaccines, culminating in his 2005 article "Deadly Immunity," published in Rolling Stone and Salon.
The piece alleged a government cover-up of vaccine risks—claims widely debunked and later retracted, yet it thrust Kennedy into the vanguard of vaccine skepticism.
In 2016, he founded Children’s Health Defense (CHD), an organization focused on addressing what it describes as an "epidemic" of childhood illnesses, including autism, which Kennedy controversially ties to vaccines despite overwhelming scientific evidence to the contrary.
CHD has since emerged as a potent force, using lawsuits, public outreach, and digital platforms to challenge vaccine policies and champion medical freedom. During the COVID-19 pandemic, Kennedy and CHD intensified their efforts, opposing mandates, questioning the FDA’s approval processes, and casting doubt on mRNA vaccine technology.
His 2021 book, The Real Anthony Fauci, accused the former NIAID director of colluding with pharmaceutical interests, becoming a bestseller despite fierce criticism from experts. Though often labeled a purveyor of misinformation, Kennedy’s knack for amplifying public distrust has undeniably shaped the discourse, pressuring the CDC into this historic policy shift.
The CDC’s Decision: What It Means
The CDC’s removal of the COVID-19 vaccine from the federal immunization schedule signifies that it is no longer a routine recommendation for the general population—a stark departure from its celebrated rollout in 2020. Several factors likely drove this change: the virus’s evolution, the vaccines’ diminishing effectiveness against transmission, and a reassessment of their risk-benefit profile amid reports of rare but serious side effects.
When first introduced, the vaccines—developed by Pfizer, Moderna, and others—boasted efficacy rates exceeding 90% against severe disease and death, a lifeline during the pandemic’s peak.
However, as variants like Delta and Omicron emerged, their ability to prevent infection and transmission waned, necessitating boosters and shifting their role to personal protection rather than herd immunity. Breakthrough infections became routine, though the vaccines continued to reduce hospitalization risks.
Survival rate data further complicates the narrative. According to CDC figures, COVID-19’s survival rate is exceptionally high for most groups:
Under 50 years old: Over 99.97% survival.
50-69 years old: Approximately 99.5% survival.
Over 70 years old: Around 94.5% survival.
These rates, critics argue, question the need for universal vaccination, particularly as natural immunity from prior infections has shown durability. For instance, a 2022 study in The New England Journal of Medicine suggested that immunity from previous COVID-19 infection could be as protective as vaccination against severe outcomes.
Meanwhile, safety concerns have grown. A 2023 study in the Journal of the American Medical Association highlighted an elevated risk of myocarditis—heart inflammation—post-vaccination, particularly in males aged 12-29, with incidence rates higher than initially estimated. For a virus posing minimal threat to healthy young people (e.g., a mortality rate of less than 0.001% in children under 12, per a 2023 Nature study), this has tilted the cost-benefit analysis for some demographics.
The decision’s implications are profound. It may signal a pivot toward individualized health policies, but it also risks undermining confidence in vaccination programs broadly, especially if misinterpreted as an admission of failure.
Reactions and Implications: Pros and Cons
The CDC’s move has polarized stakeholders, with reactions reflecting deep-seated divisions over vaccines.
Pros
Restoring Public Trust:
Advocates, including Kennedy, argue that acknowledging the vaccines’ limitations could mend frayed confidence in health agencies battered by years of scrutiny and mixed messaging.
Pushing for Better Science:
The shift might catalyze investment in long-term, rigorous studies, addressing gaps in current vaccine data and ensuring future interventions are unimpeachable.
Empowering Choice:
By stepping back from a blanket recommendation, the CDC respects individual risk assessments, aligning with calls for medical autonomy.
Cons
Declining Vaccination Rates:
Critics fear that without federal backing, uptake could drop sharply, exposing vulnerable groups—like the elderly or immunocompromised—to greater risk.
Fueling Misinformation:
The decision might be spun as proof of vaccine danger, amplifying hesitancy beyond COVID-19 to other immunizations.
Political Polarization:
Some view it as a concession to anti-vaccine pressure rather than a data-driven choice, deepening partisan rifts.
Experts weigh in diversely. Dr. Paul Offit, a pediatrician and vaccine proponent, warned, "Updating policies is fine, but we must clarify that vaccines still save lives." Conversely, Dr. Peter McCullough, a cardiologist critical of COVID-19 vaccine strategies, celebrated it as "a return to rational medicine." Public sentiment, per a 2024 Gallup poll, shows 35% of Americans now question vaccine safety broadly—up from 20% pre-pandemic—suggesting the decision’s messaging will be critical.
The Case for Better Clinical Studies and Trials
The COVID-19 vaccines’ rapid development was a scientific feat, but speed came at a cost. Emergency Use Authorizations (EUAs) truncated the usual multi-year approval process, leaving gaps in long-term safety and efficacy data. Initial trials, while robust in scale (e.g., Pfizer’s enrolled over 43,000 participants), were limited:
Short Follow-Up:
Most tracked outcomes for just two to three months, insufficient for detecting rare or delayed effects.
Narrow Focus:
They prioritized symptomatic infection over transmission or subgroup risks (e.g., pregnant women, children).
Transparency Issues:
A 2022 BMJ investigation revealed Pfizer withheld some trial data from regulators, raising ethical concerns.
Post-marketing surveillance via the Vaccine Adverse Event Reporting System (VAERS) has flagged issues like myocarditis and blood clots, but its voluntary nature complicates causation. A 2024 Lancet meta-analysis estimated serious adverse events at 1 in 10,000 doses—rare, yet significant given billions administered globally.
Kennedy and CHD have long demanded gold-standard research: randomized controlled trials for boosters, extended follow-ups, and full data disclosure. The CDC’s decision could refocus efforts on such rigor, ensuring vaccines withstand scrutiny and bolster public trust.
Informed Consent: Empowering the Individual
Informed consent—providing patients with comprehensive, unbiased information—is a cornerstone of ethical medicine. During the pandemic, mandates and societal pressure often sidelined this principle, with policies like workplace vaccine requirements leaving little room for refusal. The CDC’s shift reasserts autonomy, recognizing that a one-size-fits-all approach may not suit a virus with such varied impact.
For example, the negligible risk to healthy children (mortality <0.001%) contrasts with higher risks in the elderly (94.5% survival over 70), per CDC and Nature data. Parents and individuals deserve to weigh these stats against vaccine risks like myocarditis.
Coercion, as seen in 2021’s mandate battles, fosters resentment; choice builds cooperation. This policy tweak could pave the way for a more tailored public health model.
Big Pharma’s Role: Money, Power, and Public Health
The pharmaceutical industry’s role looms large. In 2021, Pfizer and Moderna reaped over $50 billion from COVID-19 vaccines, with profit margins topping 20%. Such financial stakes invite skepticism about motives. Historical parallels—like Purdue Pharma’s OxyContin debacle—underscore how profit can skew science and policy.
Transparency remains a sore point. The *BMJ*’s 2022 exposé showed Pfizer obscured trial data, while the FDA’s reliance on industry-funded studies has drawn fire. Regulatory capture—where ex-pharma executives populate agencies like the CDC—further muddies trust. Reforms like mandatory data releases and stricter conflict-of-interest rules could realign priorities toward public good over corporate gain.